Headaches, Migraines and Pilates
- By Peter Tziavrangos. Physiotherapist. - Peter is an APPI Pilates Instructor and Physiotherapist with a special interest in the management of Headache disorders. He has advanced training in the assessment and treatment of headaches attributed to neck dysfunction, and spends the majority of his clinical time seeing patients with these problems.
Have you ever wondered how and why neck problems can give you a headache?
Headache which is directly caused by structures within the neck is commonly referred to as Cervicogenic Headache, literally meaning headache coming from the neck. Although many people have been diagnosed with this type of headache, they often don’t really understand the physiology behind it. How can a problem in my neck, cause pain in my head?!
When we have a problem in our neck, perhaps an injury or pathology related to degenerative changes or even just constant postural loads, nerve receptors within the neck muscles and joints send messages to our brain to keep it informed of what is going on. In this case these messages are more or less telling the brain that there is a threat to the tissue. At this point, you are not yet feeling pain.
The brain then needs to decide what to do with this information, including whether it should let you know about it. In other words, your brain needs to decide whether it should make you feel pain. It is a common misconception that this process works the other way around (ie that pain messages start in the tissue and travel up to the brain). But in fact, this is how pain is felt in any other part of the body also, it isn’t actually the part of your body which you feel the pain at that is producing the pain signals, it is 100% in your brain.
Usually the brain’s accuracy at mapping the pain to the correct area of your body is pretty good. If we injure our neck, we should and do usually feel the pain at the site of the injury. But a number of factors can alter this accuracy, and in relation to Cervicogenic headache it is related to the anatomy of the nerve pathways.
So why does the head hurt?
Well in the case of Cervicogenic Headache, there is actually no injury in your head which is driving the pain process.
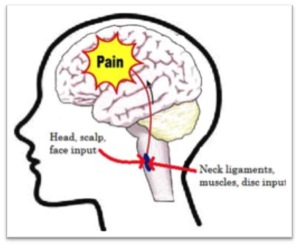
It is all to do with the pathway that the messages take on their way to the brain. The upper 3 cervical (neck) nerves from each side pass into the spinal cord, and up a tract through the brainstem (base of the brain) into an area known as the Trigemino-Cervical Nucleus (TCN). A separate set of nerves on each side of the head known as the Trigeminal nerves also connect into the same TCN. The Trigeminal nerves play a role in taking messages from the head/face to the brain, via the TCN.
The convergence of these two types of nerves (neck nerves and Trigeminal nerves) results in confusion as to where the original message came from. Essentially, the brain receives a message regarding threat to the tissues, but it can’t be sure if it came from your neck, head or face. The brain produces pain on the wrong part of the map, giving you pain in the head instead of just the neck.
…but what about Migraines?
Diagnosis of migraine usually occurs at a Doctor’s assessment, and is formulated based on the symptoms you present with. In other words, there really isn’t a medical ‘test’ for migraine. The diagnosis is traditionally made using a symptom based classification system, which was developed by the International Headache Society. Symptoms can include intense pain, sensitivity to light, dizziness and sometimes nausea and visual and sensory symptoms called auras. Once more serious causes of the symptoms (like stroke or cancer) have been ruled out medical treatment usually involves long term use of medications.
Despite how severe the symptoms might be, there usually isn’t anything serious to be found on blood tests and scans, which can be quite frustrating for the Migraine sufferer, and then to be left with the prospects of taking medications for the rest of their lives is unacceptable for some.
Interestingly, experts around the world are seeing that there are some common findings in the brains of headache sufferers even though these people may have been diagnosed with different headache types. The common findings relate to the sensitivity of the Trigemino-Cervical Nucleus (TCN) in the brainstem.
Rather than defining the different classifications of Headache (eg migraine, tension-type headache and cluster headache) as separate entities, it is thought that these are more like a spectrum or continuum of presentations. These findings are somewhat controversial as many purist Doctors strictly adhere to the older style diagnosis using a classification system only.
Our clinic has seen the benefit of the latest research and findings when applied to Migraine sufferers with neck contribution to their problem.
How can the neck contribute to migraines?
The continuum theory research has shown us that the one common thing amongst headache sufferers, is that the TCN is in a sensitised state. We also know that it may only become sensitised by a few things. One example is serotonin’s effect on the TCN and many of the drugs used to manage migraine target this.
We also know that having a neck problem also sends messages through the TCN (see further information about the anatomy of this in the Cervicogenic Headache section). If these messages relate to threat (for example from tissue damage), and are repeated chronically then this also sensitises the nucleus. This can then effectively reduce your threshold to triggers of a migraine. In other words, a problem in your neck can be contributing to your migraines!
So what do we do about it?
Obviously a thorough medical assessment is the key to ruling out any serious underlying disease or pathology, but if we have determined that there is a musculoskeletal contribution, it is important to correctly assess this in the context of a bio-psycho-social assessment.
Manual therapy can play an important role, where a skilled assessment is used to identify whether hypo-mobility of the upper cervical segments is contributing. Further to this, looking at posture of the head, neck, scapulae and thoracic spine is also crucial for long term management. Postural awareness and endurance seem to be most important and so education and specific exercise prescription (including dosage) are important. Starting with looking at motor control with cranio-cervical flexor endurance in supine and also scapular control in weight bearing gives you a good baseline to start home exercises. These can become boring very quickly though, so I find compliance with exercises and therefore outcomes improve as soon as we can progress to Pilates exercises.
Pilates
For too long, Pilates has had a reputation of just being about working on your core and getting a six pack. Although this can be an important part of a Pilates workout, it is important to note that the Pilates repertoire can cover the whole body, and that a workout should involve more than just moving or stabilising one part.
So even if I am running a class with a focus on upper quadrant training, I will always include whole body movements and exercises away from the neck and shoulders. This is also important from a loading perspective. Doing a 60 minute classes where all that is covered is upper quadrant exercises and stretches is a sure-fire way to aggravate shoulder and neck problems by overloading them.
In a class for upper quadrant problems I do ensure I cover exercises within the workout to increase thoracic mobility (with exercises like Arm Openings and Cat Stretch) and improve neck/scap motor control (with exercises like Swan Dive, Swimming in 4 point and Breast Stroke variations amongst others). The challenge is not to start the motor control at too high a level or challenge endurance-wise, and so these clients will always need to have started these exercises as part of a treatment programme 1:1.
An additional aspect of a Pilates Mat class which I feel is relevant to headache sufferers is that the concentration required throughout the class and following such specific instructions relating to movement creates an almost meditative effect. Being mindful about our movement during the class, I feel, has the ability to reduce stress levels and helps us practice ‘staying in the moment’. Further to this I have seen the added benefit of attending Mindfulness Based Stress Reduction courses in addition to having manual therapy or attending Pilates classes, and it has led to some great clinical outcomes for some of my patients.
Although there isn’t a lot of research out there looking at Neck dysfunction/Headaches and Pilates. We were encouraged to see the findings of a Pilot Study in Dublin looking at the effect of a 6 week Pilates Mat Programme on a population of chronic neck patients.
(The Effectiveness of a 6-week Pilates programme on the outcome measures in a population of chronic neck pain patients: A Pilot Study. Germaine Mallin and Susan Murphy. Journal of Bodywork and Movement Therapies, 2013).
Image: Convergence of the Trigeminal nerve and the neck nerves at the TCN.
Peter Tziavrangos
Book in to see Peter at his clinic Move Physiotherapy & Pilates in Adelaide
Website: www.movephysio.com.au
- Peter is an APPI Pilates Instructor and Physiotherapist with a special interest in the management of Headache disorders. He has advanced training in the assessment and treatment of headaches attributed to neck dysfunction, and spends the majority of his clinical time seeing patients with these problems.
Have you ever wondered how and why neck problems can give you a headache?
Headache which is directly caused by structures within the neck is commonly referred to as Cervicogenic Headache, literally meaning headache coming from the neck. Although many people have been diagnosed with this type of headache, they often don’t really understand the physiology behind it. How can a problem in my neck, cause pain in my head?!
When we have a problem in our neck, perhaps an injury or pathology related to degenerative changes or even just constant postural loads, nerve receptors within the neck muscles and joints send messages to our brain to keep it informed of what is going on. In this case these messages are more or less telling the brain that there is a threat to the tissue. At this point, you are not yet feeling pain.
The brain then needs to decide what to do with this information, including whether it should let you know about it. In other words, your brain needs to decide whether it should make you feel pain. It is a common misconception that this process works the other way around (ie that pain messages start in the tissue and travel up to the brain). But in fact, this is how pain is felt in any other part of the body also, it isn’t actually the part of your body which you feel the pain at that is producing the pain signals, it is 100% in your brain.
Usually the brain’s accuracy at mapping the pain to the correct area of your body is pretty good. If we injure our neck, we should and do usually feel the pain at the site of the injury. But a number of factors can alter this accuracy, and in relation to Cervicogenic headache it is related to the anatomy of the nerve pathways.
So why does the head hurt?
Well in the case of Cervicogenic Headache, there is actually no injury in your head which is driving the pain process.
It is all to do with the pathway that the messages take on their way to the brain. The upper 3 cervical (neck) nerves from each side pass into the spinal cord, and up a tract through the brainstem (base of the brain) into an area known as the Trigemino-Cervical Nucleus (TCN). A separate set of nerves on each side of the head known as the Trigeminal nerves also connect into the same TCN. The Trigeminal nerves play a role in taking messages from the head/face to the brain, via the TCN.
The convergence of these two types of nerves (neck nerves and Trigeminal nerves) results in confusion as to where the original message came from. Essentially, the brain receives a message regarding threat to the tissues, but it can’t be sure if it came from your neck, head or face. The brain produces pain on the wrong part of the map, giving you pain in the head instead of just the neck.
…but what about Migraines?
Diagnosis of migraine usually occurs at a Doctor’s assessment, and is formulated based on the symptoms you present with. In other words, there really isn’t a medical ‘test’ for migraine. The diagnosis is traditionally made using a symptom based classification system, which was developed by the International Headache Society. Symptoms can include intense pain, sensitivity to light, dizziness and sometimes nausea and visual and sensory symptoms called auras. Once more serious causes of the symptoms (like stroke or cancer) have been ruled out medical treatment usually involves long term use of medications.
Despite how severe the symptoms might be, there usually isn’t anything serious to be found on blood tests and scans, which can be quite frustrating for the Migraine sufferer, and then to be left with the prospects of taking medications for the rest of their lives is unacceptable for some.
Interestingly, experts around the world are seeing that there are some common findings in the brains of headache sufferers even though these people may have been diagnosed with different headache types. The common findings relate to the sensitivity of the Trigemino-Cervical Nucleus (TCN) in the brainstem.
Rather than defining the different classifications of Headache (eg migraine, tension-type headache and cluster headache) as separate entities, it is thought that these are more like a spectrum or continuum of presentations. These findings are somewhat controversial as many purist Doctors strictly adhere to the older style diagnosis using a classification system only.
Our clinic has seen the benefit of the latest research and findings when applied to Migraine sufferers with neck contribution to their problem.
How can the neck contribute to migraines?
The continuum theory research has shown us that the one common thing amongst headache sufferers, is that the TCN is in a sensitised state. We also know that it may only become sensitised by a few things. One example is serotonin’s effect on the TCN and many of the drugs used to manage migraine target this.
We also know that having a neck problem also sends messages through the TCN (see further information about the anatomy of this in the Cervicogenic Headache section). If these messages relate to threat (for example from tissue damage), and are repeated chronically then this also sensitises the nucleus. This can then effectively reduce your threshold to triggers of a migraine. In other words, a problem in your neck can be contributing to your migraines!
So what do we do about it?
Obviously a thorough medical assessment is the key to ruling out any serious underlying disease or pathology, but if we have determined that there is a musculoskeletal contribution, it is important to correctly assess this in the context of a bio-psycho-social assessment.
Manual therapy can play an important role, where a skilled assessment is used to identify whether hypo-mobility of the upper cervical segments is contributing. Further to this, looking at posture of the head, neck, scapulae and thoracic spine is also crucial for long term management. Postural awareness and endurance seem to be most important and so education and specific exercise prescription (including dosage) are important. Starting with looking at motor control with cranio-cervical flexor endurance in supine and also scapular control in weight bearing gives you a good baseline to start home exercises. These can become boring very quickly though, so I find compliance with exercises and therefore outcomes improve as soon as we can progress to Pilates exercises.
Pilates
For too long, Pilates has had a reputation of just being about working on your core and getting a six pack. Although this can be an important part of a Pilates workout, it is important to note that the Pilates repertoire can cover the whole body, and that a workout should involve more than just moving or stabilising one part.
So even if I am running a class with a focus on upper quadrant training, I will always include whole body movements and exercises away from the neck and shoulders. This is also important from a loading perspective. Doing a 60 minute classes where all that is covered is upper quadrant exercises and stretches is a sure-fire way to aggravate shoulder and neck problems by overloading them.
In a class for upper quadrant problems I do ensure I cover exercises within the workout to increase thoracic mobility (with exercises like Arm Openings and Cat Stretch) and improve neck/scap motor control (with exercises like Swan Dive, Swimming in 4 point and Breast Stroke variations amongst others). The challenge is not to start the motor control at too high a level or challenge endurance-wise, and so these clients will always need to have started these exercises as part of a treatment programme 1:1.
An additional aspect of a Pilates Mat class which I feel is relevant to headache sufferers is that the concentration required throughout the class and following such specific instructions relating to movement creates an almost meditative effect. Being mindful about our movement during the class, I feel, has the ability to reduce stress levels and helps us practice ‘staying in the moment’. Further to this I have seen the added benefit of attending Mindfulness Based Stress Reduction courses in addition to having manual therapy or attending Pilates classes, and it has led to some great clinical outcomes for some of my patients.
Although there isn’t a lot of research out there looking at Neck dysfunction/Headaches and Pilates. We were encouraged to see the findings of a Pilot Study in Dublin looking at the effect of a 6 week Pilates Mat Programme on a population of chronic neck patients.
(The Effectiveness of a 6-week Pilates programme on the outcome measures in a population of chronic neck pain patients: A Pilot Study. Germaine Mallin and Susan Murphy. Journal of Bodywork and Movement Therapies, 2013).
Image: Convergence of the Trigeminal nerve and the neck nerves at the TCN.
Peter Tziavrangos
Book in to see Peter at his clinic Move Physiotherapy & Pilates in Adelaide
Website: www.movephysio.com.au
 - Peter is an APPI Pilates Instructor and Physiotherapist with a special interest in the management of Headache disorders. He has advanced training in the assessment and treatment of headaches attributed to neck dysfunction, and spends the majority of his clinical time seeing patients with these problems.
Have you ever wondered how and why neck problems can give you a headache?
Headache which is directly caused by structures within the neck is commonly referred to as Cervicogenic Headache, literally meaning headache coming from the neck. Although many people have been diagnosed with this type of headache, they often don’t really understand the physiology behind it. How can a problem in my neck, cause pain in my head?!
When we have a problem in our neck, perhaps an injury or pathology related to degenerative changes or even just constant postural loads, nerve receptors within the neck muscles and joints send messages to our brain to keep it informed of what is going on. In this case these messages are more or less telling the brain that there is a threat to the tissue. At this point, you are not yet feeling pain.
The brain then needs to decide what to do with this information, including whether it should let you know about it. In other words, your brain needs to decide whether it should make you feel pain. It is a common misconception that this process works the other way around (ie that pain messages start in the tissue and travel up to the brain). But in fact, this is how pain is felt in any other part of the body also, it isn’t actually the part of your body which you feel the pain at that is producing the pain signals, it is 100% in your brain.
Usually the brain’s accuracy at mapping the pain to the correct area of your body is pretty good. If we injure our neck, we should and do usually feel the pain at the site of the injury. But a number of factors can alter this accuracy, and in relation to Cervicogenic headache it is related to the anatomy of the nerve pathways.
So why does the head hurt?
Well in the case of Cervicogenic Headache, there is actually no injury in your head which is driving the pain process.
It is all to do with the pathway that the messages take on their way to the brain. The upper 3 cervical (neck) nerves from each side pass into the spinal cord, and up a tract through the brainstem (base of the brain) into an area known as the Trigemino-Cervical Nucleus (TCN). A separate set of nerves on each side of the head known as the Trigeminal nerves also connect into the same TCN. The Trigeminal nerves play a role in taking messages from the head/face to the brain, via the TCN.
The convergence of these two types of nerves (neck nerves and Trigeminal nerves) results in confusion as to where the original message came from. Essentially, the brain receives a message regarding threat to the tissues, but it can’t be sure if it came from your neck, head or face. The brain produces pain on the wrong part of the map, giving you pain in the head instead of just the neck.
…but what about Migraines?
Diagnosis of migraine usually occurs at a Doctor’s assessment, and is formulated based on the symptoms you present with. In other words, there really isn’t a medical ‘test’ for migraine. The diagnosis is traditionally made using a symptom based classification system, which was developed by the International Headache Society. Symptoms can include intense pain, sensitivity to light, dizziness and sometimes nausea and visual and sensory symptoms called auras. Once more serious causes of the symptoms (like stroke or cancer) have been ruled out medical treatment usually involves long term use of medications.
Despite how severe the symptoms might be, there usually isn’t anything serious to be found on blood tests and scans, which can be quite frustrating for the Migraine sufferer, and then to be left with the prospects of taking medications for the rest of their lives is unacceptable for some.
Interestingly, experts around the world are seeing that there are some common findings in the brains of headache sufferers even though these people may have been diagnosed with different headache types. The common findings relate to the sensitivity of the Trigemino-Cervical Nucleus (TCN) in the brainstem.
Rather than defining the different classifications of Headache (eg migraine, tension-type headache and cluster headache) as separate entities, it is thought that these are more like a spectrum or continuum of presentations. These findings are somewhat controversial as many purist Doctors strictly adhere to the older style diagnosis using a classification system only.
Our clinic has seen the benefit of the latest research and findings when applied to Migraine sufferers with neck contribution to their problem.
How can the neck contribute to migraines?
The continuum theory research has shown us that the one common thing amongst headache sufferers, is that the TCN is in a sensitised state. We also know that it may only become sensitised by a few things. One example is serotonin’s effect on the TCN and many of the drugs used to manage migraine target this.
We also know that having a neck problem also sends messages through the TCN (see further information about the anatomy of this in the Cervicogenic Headache section). If these messages relate to threat (for example from tissue damage), and are repeated chronically then this also sensitises the nucleus. This can then effectively reduce your threshold to triggers of a migraine. In other words, a problem in your neck can be contributing to your migraines!
So what do we do about it?
Obviously a thorough medical assessment is the key to ruling out any serious underlying disease or pathology, but if we have determined that there is a musculoskeletal contribution, it is important to correctly assess this in the context of a bio-psycho-social assessment.
Manual therapy can play an important role, where a skilled assessment is used to identify whether hypo-mobility of the upper cervical segments is contributing. Further to this, looking at posture of the head, neck, scapulae and thoracic spine is also crucial for long term management. Postural awareness and endurance seem to be most important and so education and specific exercise prescription (including dosage) are important. Starting with looking at motor control with cranio-cervical flexor endurance in supine and also scapular control in weight bearing gives you a good baseline to start home exercises. These can become boring very quickly though, so I find compliance with exercises and therefore outcomes improve as soon as we can progress to Pilates exercises.
Pilates
For too long, Pilates has had a reputation of just being about working on your core and getting a six pack. Although this can be an important part of a Pilates workout, it is important to note that the Pilates repertoire can cover the whole body, and that a workout should involve more than just moving or stabilising one part.
So even if I am running a class with a focus on upper quadrant training, I will always include whole body movements and exercises away from the neck and shoulders. This is also important from a loading perspective. Doing a 60 minute classes where all that is covered is upper quadrant exercises and stretches is a sure-fire way to aggravate shoulder and neck problems by overloading them.
In a class for upper quadrant problems I do ensure I cover exercises within the workout to increase thoracic mobility (with exercises like Arm Openings and Cat Stretch) and improve neck/scap motor control (with exercises like Swan Dive, Swimming in 4 point and Breast Stroke variations amongst others). The challenge is not to start the motor control at too high a level or challenge endurance-wise, and so these clients will always need to have started these exercises as part of a treatment programme 1:1.
An additional aspect of a Pilates Mat class which I feel is relevant to headache sufferers is that the concentration required throughout the class and following such specific instructions relating to movement creates an almost meditative effect. Being mindful about our movement during the class, I feel, has the ability to reduce stress levels and helps us practice ‘staying in the moment’. Further to this I have seen the added benefit of attending Mindfulness Based Stress Reduction courses in addition to having manual therapy or attending Pilates classes, and it has led to some great clinical outcomes for some of my patients.
Although there isn’t a lot of research out there looking at Neck dysfunction/Headaches and Pilates. We were encouraged to see the findings of a Pilot Study in Dublin looking at the effect of a 6 week Pilates Mat Programme on a population of chronic neck patients.
(The Effectiveness of a 6-week Pilates programme on the outcome measures in a population of chronic neck pain patients: A Pilot Study. Germaine Mallin and Susan Murphy. Journal of Bodywork and Movement Therapies, 2013).
Image: Convergence of the Trigeminal nerve and the neck nerves at the TCN.
Peter Tziavrangos
Book in to see Peter at his clinic Move Physiotherapy & Pilates in Adelaide
Website: www.movephysio.com.au
- Peter is an APPI Pilates Instructor and Physiotherapist with a special interest in the management of Headache disorders. He has advanced training in the assessment and treatment of headaches attributed to neck dysfunction, and spends the majority of his clinical time seeing patients with these problems.
Have you ever wondered how and why neck problems can give you a headache?
Headache which is directly caused by structures within the neck is commonly referred to as Cervicogenic Headache, literally meaning headache coming from the neck. Although many people have been diagnosed with this type of headache, they often don’t really understand the physiology behind it. How can a problem in my neck, cause pain in my head?!
When we have a problem in our neck, perhaps an injury or pathology related to degenerative changes or even just constant postural loads, nerve receptors within the neck muscles and joints send messages to our brain to keep it informed of what is going on. In this case these messages are more or less telling the brain that there is a threat to the tissue. At this point, you are not yet feeling pain.
The brain then needs to decide what to do with this information, including whether it should let you know about it. In other words, your brain needs to decide whether it should make you feel pain. It is a common misconception that this process works the other way around (ie that pain messages start in the tissue and travel up to the brain). But in fact, this is how pain is felt in any other part of the body also, it isn’t actually the part of your body which you feel the pain at that is producing the pain signals, it is 100% in your brain.
Usually the brain’s accuracy at mapping the pain to the correct area of your body is pretty good. If we injure our neck, we should and do usually feel the pain at the site of the injury. But a number of factors can alter this accuracy, and in relation to Cervicogenic headache it is related to the anatomy of the nerve pathways.
So why does the head hurt?
Well in the case of Cervicogenic Headache, there is actually no injury in your head which is driving the pain process.
It is all to do with the pathway that the messages take on their way to the brain. The upper 3 cervical (neck) nerves from each side pass into the spinal cord, and up a tract through the brainstem (base of the brain) into an area known as the Trigemino-Cervical Nucleus (TCN). A separate set of nerves on each side of the head known as the Trigeminal nerves also connect into the same TCN. The Trigeminal nerves play a role in taking messages from the head/face to the brain, via the TCN.
The convergence of these two types of nerves (neck nerves and Trigeminal nerves) results in confusion as to where the original message came from. Essentially, the brain receives a message regarding threat to the tissues, but it can’t be sure if it came from your neck, head or face. The brain produces pain on the wrong part of the map, giving you pain in the head instead of just the neck.
…but what about Migraines?
Diagnosis of migraine usually occurs at a Doctor’s assessment, and is formulated based on the symptoms you present with. In other words, there really isn’t a medical ‘test’ for migraine. The diagnosis is traditionally made using a symptom based classification system, which was developed by the International Headache Society. Symptoms can include intense pain, sensitivity to light, dizziness and sometimes nausea and visual and sensory symptoms called auras. Once more serious causes of the symptoms (like stroke or cancer) have been ruled out medical treatment usually involves long term use of medications.
Despite how severe the symptoms might be, there usually isn’t anything serious to be found on blood tests and scans, which can be quite frustrating for the Migraine sufferer, and then to be left with the prospects of taking medications for the rest of their lives is unacceptable for some.
Interestingly, experts around the world are seeing that there are some common findings in the brains of headache sufferers even though these people may have been diagnosed with different headache types. The common findings relate to the sensitivity of the Trigemino-Cervical Nucleus (TCN) in the brainstem.
Rather than defining the different classifications of Headache (eg migraine, tension-type headache and cluster headache) as separate entities, it is thought that these are more like a spectrum or continuum of presentations. These findings are somewhat controversial as many purist Doctors strictly adhere to the older style diagnosis using a classification system only.
Our clinic has seen the benefit of the latest research and findings when applied to Migraine sufferers with neck contribution to their problem.
How can the neck contribute to migraines?
The continuum theory research has shown us that the one common thing amongst headache sufferers, is that the TCN is in a sensitised state. We also know that it may only become sensitised by a few things. One example is serotonin’s effect on the TCN and many of the drugs used to manage migraine target this.
We also know that having a neck problem also sends messages through the TCN (see further information about the anatomy of this in the Cervicogenic Headache section). If these messages relate to threat (for example from tissue damage), and are repeated chronically then this also sensitises the nucleus. This can then effectively reduce your threshold to triggers of a migraine. In other words, a problem in your neck can be contributing to your migraines!
So what do we do about it?
Obviously a thorough medical assessment is the key to ruling out any serious underlying disease or pathology, but if we have determined that there is a musculoskeletal contribution, it is important to correctly assess this in the context of a bio-psycho-social assessment.
Manual therapy can play an important role, where a skilled assessment is used to identify whether hypo-mobility of the upper cervical segments is contributing. Further to this, looking at posture of the head, neck, scapulae and thoracic spine is also crucial for long term management. Postural awareness and endurance seem to be most important and so education and specific exercise prescription (including dosage) are important. Starting with looking at motor control with cranio-cervical flexor endurance in supine and also scapular control in weight bearing gives you a good baseline to start home exercises. These can become boring very quickly though, so I find compliance with exercises and therefore outcomes improve as soon as we can progress to Pilates exercises.
Pilates
For too long, Pilates has had a reputation of just being about working on your core and getting a six pack. Although this can be an important part of a Pilates workout, it is important to note that the Pilates repertoire can cover the whole body, and that a workout should involve more than just moving or stabilising one part.
So even if I am running a class with a focus on upper quadrant training, I will always include whole body movements and exercises away from the neck and shoulders. This is also important from a loading perspective. Doing a 60 minute classes where all that is covered is upper quadrant exercises and stretches is a sure-fire way to aggravate shoulder and neck problems by overloading them.
In a class for upper quadrant problems I do ensure I cover exercises within the workout to increase thoracic mobility (with exercises like Arm Openings and Cat Stretch) and improve neck/scap motor control (with exercises like Swan Dive, Swimming in 4 point and Breast Stroke variations amongst others). The challenge is not to start the motor control at too high a level or challenge endurance-wise, and so these clients will always need to have started these exercises as part of a treatment programme 1:1.
An additional aspect of a Pilates Mat class which I feel is relevant to headache sufferers is that the concentration required throughout the class and following such specific instructions relating to movement creates an almost meditative effect. Being mindful about our movement during the class, I feel, has the ability to reduce stress levels and helps us practice ‘staying in the moment’. Further to this I have seen the added benefit of attending Mindfulness Based Stress Reduction courses in addition to having manual therapy or attending Pilates classes, and it has led to some great clinical outcomes for some of my patients.
Although there isn’t a lot of research out there looking at Neck dysfunction/Headaches and Pilates. We were encouraged to see the findings of a Pilot Study in Dublin looking at the effect of a 6 week Pilates Mat Programme on a population of chronic neck patients.
(The Effectiveness of a 6-week Pilates programme on the outcome measures in a population of chronic neck pain patients: A Pilot Study. Germaine Mallin and Susan Murphy. Journal of Bodywork and Movement Therapies, 2013).
Image: Convergence of the Trigeminal nerve and the neck nerves at the TCN.
Peter Tziavrangos
Book in to see Peter at his clinic Move Physiotherapy & Pilates in Adelaide
Website: www.movephysio.com.au